[h=1]Stem cells found in blood vessels can help make muscle[/h]
<fieldset class="fieldgroup group-summary" style="padding: 1em; margin: 1em 0px; clear: left; width: 707px; overflow: visible; border: 1px solid rgb(204, 204, 204); "><legend style="padding: 0px; margin: 0px; font-size: 1.7em; font-family: Georgia, 'Times New Roman', Times, serif; letter-spacing: 0px; ">Summary of research</legend>

Research has shown for the first time that a non-muscle type of cell can switch to help make muscle during normal growth. These cells, called pericytes, which are normally found on small blood vessels, were shown to also make both muscle fibres and muscle stem cells. Whilst it has been shown that in extreme situations pericytes can contribute to muscle repair, it was not known whether this was also part of natural muscle growth. This finding is important because it means that normally, there is a signal which ‘tells’ the pericytes to make muscle. We don’t yet know what this signal is but, once we do, it could be used to help repair damaged muscle after injury or disease.
</fieldset>[h=2]What is the idea behind this study?[/h]When muscles are damaged after injury or in disorders such as muscular dystrophy, specialised muscle stem cells or ‘satellite cells’ repair them by making new muscle. This process is called ‘regeneration’. It has recently been shown that during extreme regeneration in muscle, other stem cells have the potential to contribute to muscle repair. It is thought that this could be when the satellite cells are overwhelmed and cannot make enough muscle. One of the other stem cells shown to repair extensively damaged muscle is pericytes.
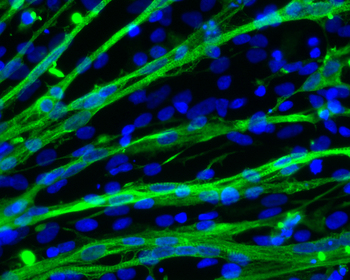
A pericyte is a type of stem cell which sits wrapped around small blood vessels called capillaries. Capillaries with connected pericytes are found throughout long fibres of muscle tissue providing nutrients and oxygen, and allowing the muscle to function normally. This results in many pericytes being found next to satellite cells inside a muscle.
There are currently no cures for muscular disorders, and a major hope for the future is stem cell therapies. This would involve giving the individual healthy stem cells, which would repair the damaged muscle both immediately, and when future damage occurred.
Although it seems that pericyte cells could have great potential in future therapies, it was not known whether their apparent muscle-making ability was only seen after major injuries, or if it naturally occurred. The idea of this study was to determine whether or not pericytes contribute to normal muscle growth.
[h=2]What did this study show?[/h]In this study, the scientists from San Raffaele Scientific Institute, Milan followed a subset of pericytes producing a protein called Alkaline phosphatase (AP) in mice. To see these cells easily, they marked the AP-producing cells. Straight after marking, these cells were only found around the blood vessels. This proved that they were marking cells which weren’t originally found in the muscle tissue.
To see whether the AP producing pericytes helped to make muscle during growth, they marked the AP-producing pericytes of young mice and waited until adulthood. They saw that over time muscle fibres and satellite cells also became marked. This meant that the marked pericytes were able to change the type of cells they were to become muscle and muscle-specific stem cells. When they did the same experiment in fully grown mice, hardly any muscle became marked, which showed that during maintenance the pericytes weren’t required. They also noticed that when muscles were regenerating, after injury or in a model of Duchenne muscular dystrophy, the number of marked muscle fibres increased.
The researchers tested the muscle-making potential of the switched pericytes by culturing them in a laboratory. They saw that 30% of cells spontaneously made muscle, and that they behaved as normal satellite cells.
These experiments show that there is a balance. During normal maintenance, the satellite cells alone repair damaged muscle. However, when lots of muscle is required – during growth and major repair – AP-producing pericytes help satellite cells to make extra muscle.
[h=2]What does this mean for patients?[/h]Transplanting healthy muscle-making stem cells in the clinic has great potential, but there are several hurdles to overcome. The current issue with the main muscle stem cell – satellite cells – is how to put them into a patients muscle. If they are injected into the bloodstream, they do not efficiently travel to affected muscles. Therefore satellite cells need to be injected into each affected muscle, which is not very efficient. The benefit of using pericytes is that being a blood vessel-associated cell, they can be injected into the blood and find damaged muscle. In fact, human clinical trials in Italy have already started where they are injecting healthy mesoangioblasts, the in vitro expanded cell population derived from pericytes into boys with Duchenne muscular dystrophy (DMD). However, this is at the stage where they are testing the safety of this, and it will be several years until this is completed.
The knowledge from this paper that pericytes normally contribute to muscle growth and the satellite cell population is very important, especially as it showed for the first time that AP-producing pericytes in growing mice switched cell-type to become satellite cells. It is not known what ‘told’ the cells to switch, but finding this out would be valuable for future clinical applications. This is because once we know what this signal is, scientists could use it to maximise the muscle-making potential of pericytes. An example of this would be in muscular dystrophy, where the individual’s satellite cells do not function correctly, so cannot repair damaged muscle. Healthy pericytes could be given the signal to become satellite cells before being injected. Once they travel to the damaged muscles, as well as repairing them, they could provide a new population of satellite cells to repair future damage. This would increase the efficiency of the therapy, providing that it is safe.
<fieldset class="fieldgroup group-summary" style="padding: 1em; margin: 1em 0px; clear: left; width: 707px; overflow: visible; border: 1px solid rgb(204, 204, 204); "><legend style="padding: 0px; margin: 0px; font-size: 1.7em; font-family: Georgia, 'Times New Roman', Times, serif; letter-spacing: 0px; ">Summary of research</legend>

Research has shown for the first time that a non-muscle type of cell can switch to help make muscle during normal growth. These cells, called pericytes, which are normally found on small blood vessels, were shown to also make both muscle fibres and muscle stem cells. Whilst it has been shown that in extreme situations pericytes can contribute to muscle repair, it was not known whether this was also part of natural muscle growth. This finding is important because it means that normally, there is a signal which ‘tells’ the pericytes to make muscle. We don’t yet know what this signal is but, once we do, it could be used to help repair damaged muscle after injury or disease.
</fieldset>[h=2]What is the idea behind this study?[/h]When muscles are damaged after injury or in disorders such as muscular dystrophy, specialised muscle stem cells or ‘satellite cells’ repair them by making new muscle. This process is called ‘regeneration’. It has recently been shown that during extreme regeneration in muscle, other stem cells have the potential to contribute to muscle repair. It is thought that this could be when the satellite cells are overwhelmed and cannot make enough muscle. One of the other stem cells shown to repair extensively damaged muscle is pericytes.
A pericyte is a type of stem cell which sits wrapped around small blood vessels called capillaries. Capillaries with connected pericytes are found throughout long fibres of muscle tissue providing nutrients and oxygen, and allowing the muscle to function normally. This results in many pericytes being found next to satellite cells inside a muscle.
There are currently no cures for muscular disorders, and a major hope for the future is stem cell therapies. This would involve giving the individual healthy stem cells, which would repair the damaged muscle both immediately, and when future damage occurred.
Although it seems that pericyte cells could have great potential in future therapies, it was not known whether their apparent muscle-making ability was only seen after major injuries, or if it naturally occurred. The idea of this study was to determine whether or not pericytes contribute to normal muscle growth.
[h=2]What did this study show?[/h]In this study, the scientists from San Raffaele Scientific Institute, Milan followed a subset of pericytes producing a protein called Alkaline phosphatase (AP) in mice. To see these cells easily, they marked the AP-producing cells. Straight after marking, these cells were only found around the blood vessels. This proved that they were marking cells which weren’t originally found in the muscle tissue.
To see whether the AP producing pericytes helped to make muscle during growth, they marked the AP-producing pericytes of young mice and waited until adulthood. They saw that over time muscle fibres and satellite cells also became marked. This meant that the marked pericytes were able to change the type of cells they were to become muscle and muscle-specific stem cells. When they did the same experiment in fully grown mice, hardly any muscle became marked, which showed that during maintenance the pericytes weren’t required. They also noticed that when muscles were regenerating, after injury or in a model of Duchenne muscular dystrophy, the number of marked muscle fibres increased.
The researchers tested the muscle-making potential of the switched pericytes by culturing them in a laboratory. They saw that 30% of cells spontaneously made muscle, and that they behaved as normal satellite cells.
These experiments show that there is a balance. During normal maintenance, the satellite cells alone repair damaged muscle. However, when lots of muscle is required – during growth and major repair – AP-producing pericytes help satellite cells to make extra muscle.
[h=2]What does this mean for patients?[/h]Transplanting healthy muscle-making stem cells in the clinic has great potential, but there are several hurdles to overcome. The current issue with the main muscle stem cell – satellite cells – is how to put them into a patients muscle. If they are injected into the bloodstream, they do not efficiently travel to affected muscles. Therefore satellite cells need to be injected into each affected muscle, which is not very efficient. The benefit of using pericytes is that being a blood vessel-associated cell, they can be injected into the blood and find damaged muscle. In fact, human clinical trials in Italy have already started where they are injecting healthy mesoangioblasts, the in vitro expanded cell population derived from pericytes into boys with Duchenne muscular dystrophy (DMD). However, this is at the stage where they are testing the safety of this, and it will be several years until this is completed.
The knowledge from this paper that pericytes normally contribute to muscle growth and the satellite cell population is very important, especially as it showed for the first time that AP-producing pericytes in growing mice switched cell-type to become satellite cells. It is not known what ‘told’ the cells to switch, but finding this out would be valuable for future clinical applications. This is because once we know what this signal is, scientists could use it to maximise the muscle-making potential of pericytes. An example of this would be in muscular dystrophy, where the individual’s satellite cells do not function correctly, so cannot repair damaged muscle. Healthy pericytes could be given the signal to become satellite cells before being injected. Once they travel to the damaged muscles, as well as repairing them, they could provide a new population of satellite cells to repair future damage. This would increase the efficiency of the therapy, providing that it is safe.